April 24, 2020
Posted by:
IEPA
By Avshalom Caspi and Terrie Moffitt
New research just published in JAMA Online reports on results from the Dunedin Study that challenges the current diagnostic paradigm for mental ill-health. We asked the authors to provide an overview of this landmark study and share potential implications for future research and mental health practice.
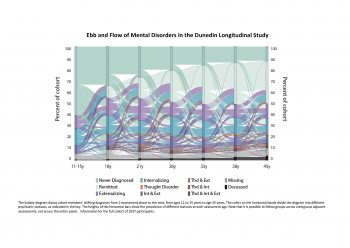
Our recent paper “Longitudinal Assessment of Mental Health Disorders and Comorbidities Across 4 Decades Among Participants in the Dunedin Birth Cohort Study” reports data from the Dunedin Longitudinal Study in New Zealand, through which we tracked 17 mental health conditions–diagnosed according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders (DSM)–with repeated standardized psychiatric assessments from age 11 to age 45, creating a detailed time series of mental health disorder life-histories.
The primary finding from the study is that over 4 decades, individuals experience many changing condition types, shifting between internalizing, externalizing, and/or thought disorder families. People seldom ‘get’ one mental health condition and keep it. Every condition predicted significantly increased risk for every other mental health condition.
Our findings indicated that, better than any particular diagnosis, three parameters described each person’s mental health: (a) age of onset, (b) duration of symptom history, and (c) number of different kinds of comorbid disorder symptoms in a life. People with younger onset of symptoms, more years with symptoms, and more different kinds of symptoms tended to be the same people. These people also had more indicators of poor brain health at age 3, steeper child-to-adult cognitive decline, and older brain-age on structural MRI at midlife.
This finding accounts for discoveries emerging from genetics and in neuroscience: Different mental health conditions share the same etiological factors in genome and brain. It should not be surprising that different mental health conditions have the same causes, because our research shows that the same person, if tracked over years, has multiple different mental health conditions. Our findings are buttressed by a companion study of decades of the Danish psychiatric register, which also found that most patients shift diagnoses, and every condition predicts increased risk for every other disorder
This finding cautions against over-reliance on etiological theories, research hypotheses, and clinical protocols that are specific to one diagnosis. Studying mental health conditions one at a time does not accurately represent most people’s lived experience of shifting across different disorders over time. Studying one condition one at a time may mislead about specificity and hide transdiagnostic discoveries from view. There is a need for measurement instruments that capture shared liability to shifting conditions across the life course in order to make discoveries more efficiently. There is also a need to develop transdiagnostic treatments that can prevent many different mental health conditions.
Access the full paper: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2764602
The figures are also available as Powerpoint slides, if you are interested. Please visit: https://moffittcaspi.trinity.duke.edu/publications